“Here are your choices,” the oncologist said. He was a young, blue-eyed man and the head of oncology at UCSD.
He flung statistics at me: “You have a 65% chance of being alive in ten years if you undergo surgery alone. That number bumps up to 75% with chemotherapy and up another ten or so with radiation and hormone therapy after that.” He smiled under his mask, hands clasped and relaxed.
“Can I choose none of the above?” I asked.
“Sure, you can walk off into the sunset. Some do. We call them lost to care. I wouldn’t advise it.”
My English major brain tried to compute these statistics about my own death. My pause was very long though peppered with comments from others. I had my team on Facetime; Mom, Dad, Sister, and Husband Ari. I didn’t really hear their questions but interrupted with my own.
“So the chance I’d be alive in ten years is about 85%?”
“Well, none of us really know if we have an 85% chance of being alive in ten years,” he said, all reassurance. I didn’t know whether to laugh or cry at that pronouncement so I did neither.
“I’ll take all three,” I said as if ordering donuts instead of deadly medications.
I chose to start with AC, the hardest one, otherwise known as The Red Devil for its color. It’s a combination of two chemotherapy drugs: doxorubicin (also known as Adriamycin) and cyclophosphamide. I would have four sessions of AC spread out every two weeks, so a total of two months. I would lose the hair on my head and on my body.
I dreaded this like nothing else I have ever dreaded in my life. My friends who went through the same thing said it wasn’t so bad for them, they could still take their kids to toddler classes. My doctor said young people tolerate AC and Taxol well and not to worry.
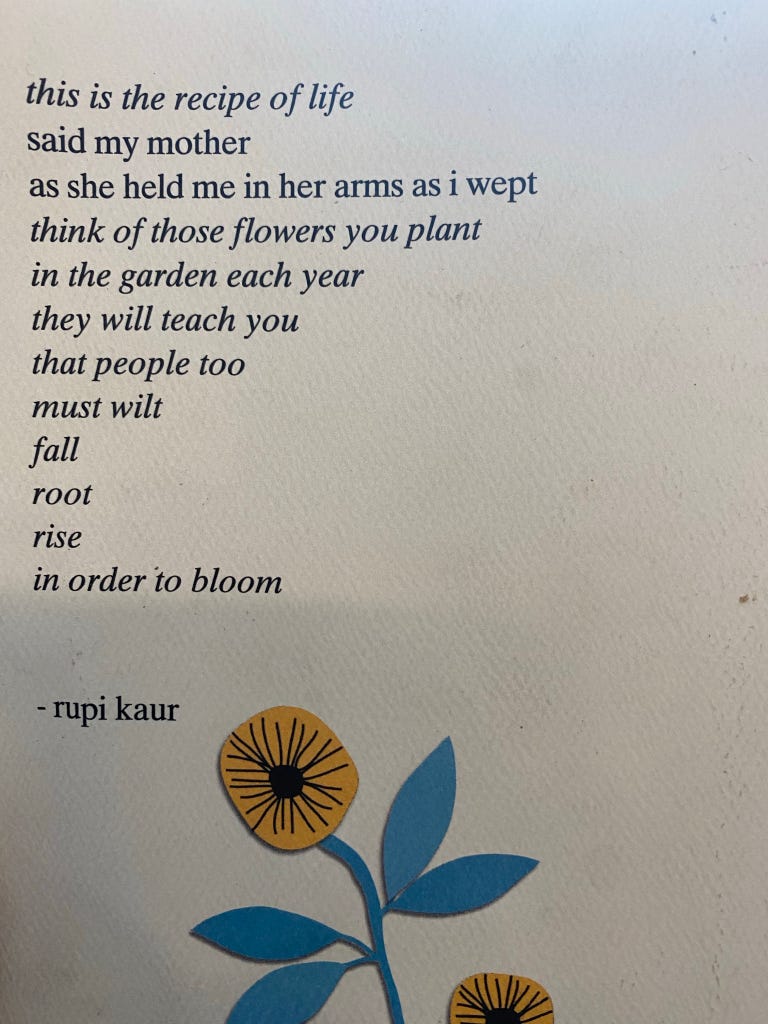
How not to worry was something I hadn’t figured out yet, though I eventually made progress on it.
First, I had to get a port installed. A port is a small round plastic and metal bulb that acts like an IV in your body. They put it in a pocket in your skin and the Chemo needle pierces the skin of your upper chest instead of an IV in your arm. It was a fantastic choice for me and I’m so glad I got one.
When I arrived at the outpatient clinic to have my port installed, they plopped a mushroom-like port in my hand. It was pretty big.

I asked for a smaller size. They gave me child’s size which made me so sad and grateful. I was in emotional overdrive.
They played classical music for me to fall asleep to though I would not go totally under. It would be like at the dentist’s office. They’d use fentanyl. When I woke up, the nurse said they had to use a lot of fentanyl to get me to go under. I left the hospital high as a kite and giggling at everyone. I learned I have a high tolerance for medications. This would help me in the long run.
I healed up at home. Anyone who has toddlers knows how hard it is to keep them off of you. No snuggles on that side. One time we were roughhousing and one of them accidentally kicked me where the port incision was healing. I screamed and probably scared them for life. More for them to talk about in their future therapy sessions.
Chemo D-Day:
I walked into the blue halls and wide windows of the hospital. I had my port, fresh and aching from two days before; a round lump in the top of my left chest, stitched like a little pocket under my skin. I had a choice of AC or Taxol but decided to start with AC, even though it was the scary one I thought of in movies when I saw a weak, bald, retching chemotherapy patient. I was about to put a harmful toxic substance in my body. I was afraid. I didn't have a choice. This was going to save my life.
I had a bunch of mantras to say: “Bad shit happens and I get through it. I’ve gotten through tough things before. I am strong. It’s very normal for people to go in and get an infusion. This is temporary. I’ll have my energy back and feel okay. The doctor weighed the risk and the benefit is worth it. I am choosing this.”
I was alone. Covid pushed out any visitors I would bring with me for a four hour session.
As a child, I had asthma and they hadn't invented the oxygen checking device that goes on your finger. Each time, they had to go into the vein to check my blood oxygen from ages 1-5. I guess you would call it medical trauma, but over the years I never lost my fear. Needles never terrified me as badly as they did now.
The nurse greeted me, a beautiful trans woman named Avi. Her flowing brown and gold locks and warm smile centered me. She gave me a window seat. She was quick, and efficient. She explained every step:
"First I'll give you anti-nausea drugs and a steroid. That will take one hour. Next you'll get the A, acedremycin which will take a few minutes, followed by the C which will take another hour.”
We chatted and chatted. I filled her in about my life. We are house shopping after living in my husband’s apartment community for ten years. I’ve been married for twelve. Met my husband in college. I have eight younger siblings. Yes, eight. No my parents are not religious, just crazy.
I might have been nervously rambling but I’m sure she was used to it.
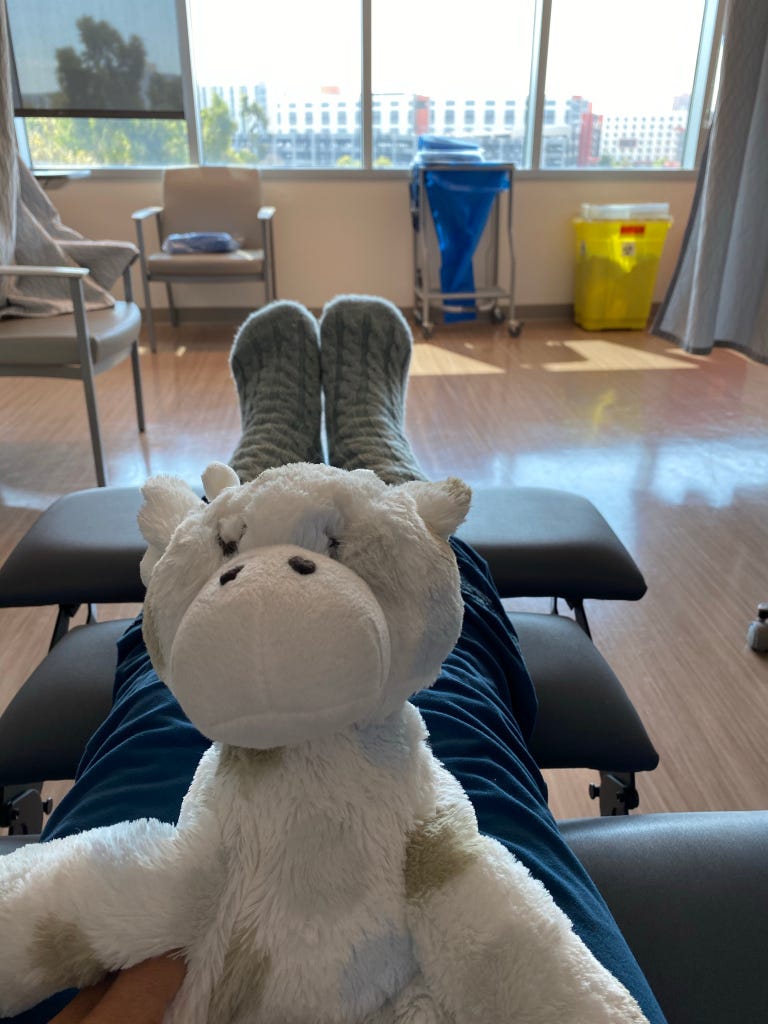
I sat with a stuffed giraffe from my dad and wore thick blue socks from my mother-in-law. Avi held up a red syringe. It was time. She sat there with me as the acedrymycin went in. I expected to feel something but didn’t. I just had to pee from all the fluids. The pee came out red.
I watched TV, read a little, and filled a coloring book. I felt hungry and asked for crackers. I ate ice to stop blisters from forming. Then it was time to go.
I left hungry from the steroids and my husband brought me a sandwich. Outside in the earth, I grounded my feet in the sand and saw God in the flowers and trees. I had done it.
The first two rounds were fine. I took the anti nausea medicine Zofran and stayed hydrated. I rested and used Metamucil for constipation. It wasn’t so bad physically. I was lucky.
The third round packed a wallop. I was more nauseous and more tired. I fretted. I flailed. I couldn’t believe this was my life now. I was so depressed. After a week of feeling tired and down, I started to feel better. My mood lifted. I can do this. I reviewed my mantras. I danced Ballet every day, even for just ten minutes.
Day by day, I took things as they came. I can beat cancer. I actually felt it stinging as it worked in my right breast and armpit.
Abraxane:
Taxol was much less of a powerhouse, everyone said. I had hope of breezing through it. I had gotten through AC. I had beaten the Red Devil.
Except, Taxol wasn’t easier. I was allergic to it.
My first time on Taxol, I sat for twenty minutes coloring in a Jane Austen coloring book. I felt a tickle in my throat, a headache, and dizziness. I pushed the nurse button. Stephanie came and gave me some Benadryl. She sat with me and watched me. Then my throat started to close. I was going into anaphylactic shock.
The nurse was amazing. Stephanie gave me more Benadryl and a steroid through my port and when it wasn’t working after a few minutes, hit me with an Epipen. I didn’t even feel it in my thigh. I calmed down. I got up, heartbeat racing from stress and the Epi. I looked out the window into the trees and thanked God I was alive.
Four strong EMTs came up to load me on a gurney to their ambulance and drive me to the ER. Why couldn’t I just walk there from hospital to the same hospital 20 feet away? They explained that when it was a separate building without a connecting corridor, you had to be driven there. I have no idea why, but suspect it has something to do with liability.
They drove me less than one minute to UCSD’s emergency room. It was COVID but I called Ari, my husband, to meet me there anyway. He saw me outside the side entrance and rushed over. I yanked his hand onto the gurney and he wheeled me along with the EMTS, through check-in and straight to a room. Ari’s blue shirt camouflaged him with the blue nurses’ scrubs, his blue eyes were nervous at being in an ER during COVID. A patient around the corner was on a ventilator. I think we are the only people who went into the ER together during COVID.
Thankfully, I was fine. They sat and observed me for a few hours and then I went home.
It took real courage to try another drug and walk into the Koman center again.
The oncologist had another drug, Abraxane, that would work the same as Taxol. It camouflaged the Taxane, poison derived from a tree, in a binding that looked like fat cells. I am allergic to grass. Of course I’d be allergic to poison from a tree. 20% of people are allergic to Taxol. Only 4% are allergic to Abraxane.
Why not start with the better, less allergic drug? Insurance doesn’t cover it unless you try and fail Taxol. Fail, as in go into anaphylactic shock and almost die.
Getting Through It
My kids gave me a new stuffy for each visit, hugs and a cheer: “Go mommy, go!”
To get through this, the hardest thing in my life, I tried new things: Grounding, Therapy, Reiki, Young Survivor’s Groups, Cancer Zumba.
Most of all, the support of my loving husband helped me get through this. His warmth, humor, and strength reminded me of my own. I am not a victim. I am choosing to fight.
I brought donuts to my final chemotherapy round. I danced to music during it. I visited other patients, some happy, some struggling, all just as courageous as I was to walk in there.
I left that final chemotherapy round with applause from the nurses and a feeling of hope that carried me out. They told me to come back and visit, to tell them how I’m doing.
I am stronger than I thought.





Beautifully written! Thanks for sharing your journey and the things that got you through it. You are so strong. Love you!
Oh, Dahlia, what a beautiful testament to your strength! I, too, did my chemo at UCSD, so was right there in thought with you, as you went through the many steps. Your husband sounds like mine. A great supporter who let me know he was there for the entire process. You are one brave woman and I’m glad you are through the worst. I’m sending you a HUGE virtual hug and can’t wait until I can see you in person! (Btw, I was an English major, too)